
619-419-0901

619-419-0901
Transcranial Magnetic Stimulation: An Effective Noninvasive Therapy
For centuries, clinicians and neuroscientists have dreamed of a method to stimulate the brain without the need for anesthesia or surgery. Several decades ago, Penfield and Perot demonstrated how electrical stimulation could impact patients in an open craniotomy, which served as a first step in thinking about various stimulation techniques.1,2
Transcranial Magnetic Stimulation (TMS) may be the answer to the dream of thousands of specialists by stimulating, noninvasively, the brain and nerve structures in awake adults. In addition, it may be the key to understanding brain-behavior relationships. However, we must keep in mind that our knowledge of TMS remains limited because it has been only a few decades since its discovery and application.
Multiple studies are still needed to understand the exact mechanisms behind TMS, since the parameters, such as intensity and frequency, vary for each person. Even so, today large organizations, such as the FDA, have approved its use for certain pathologies, which definitely supports the belief in the potential of TMS. This article is a compact overview of the operation and application of TMS.
What Is Transcranial Magnetic Stimulation?
In short, it is a non-invasive neurophysiological technique that can stimulate the human brain through the intact skull, without producing significant discomfort. In another era, we would call it a miracle. However, the lack of knowledge about its exact mechanisms takes us a bit further away from this eponymous.
It was discovered and developed by Barker and colleagues in 19853 and has been used in healthy and psychiatrically disturbed patients to explore their cortical functions. Some studies (even old ones) have tried to demonstrate an early therapeutic effect. Most of these studies focused on the primary motor cortex, although much attention was also diverted to depression, where it appears to be quite effective.4
Simply put, TMS uses magnetic stimulators that consist of small capacitors that discharge currents of extremely short duration through an induction coil placed on the scalp5. The idea is to create a magnetic field from the current that passes through the brain perpendicularly and reaches values up to 3 Tesla. In this process, part of the current is displaced and creates a second side (secondary electric current/Eddy) in the brain, which also has some effect.
Due to the short duration of the original current, the intensity of the magnetic field decreases rapidly and does not allow it to reach long distances. Therefore, the effect is thought to be limited to the cortex and part of the subcortical white matter.6
The secret is in varying the intensity and frequency of the impulses through the coil to achieve diverse stimulations and readings of the brain’s functioning. These are the patterns that are still under investigation, however, we know enough to exert effects in various brain sectors and record them.
For example, stimulation in the primary motor cortex may act as an inhibitor of the corticospinal pathway responsible for muscle activation on the contralateral side of the body. This can be recorded as a small “twitch” using electromyography. This is the potential evoked motor (MEP).
If we do not use a single impulse, but vary the amount, and use even pulses through the coil, we can record the inhibition and excitation of the muscle fibers, thus recording the functioning of the corresponding circuits. There is a whole range of possibilities with the TMS. We can create short or long repetitive pulses (rTMS), even regular or with a specific pattern in certain areas of the cortex.
However, perhaps most interestingly, TMS can cause long-term changes by creating specific protocols. But how is it maintained? Well, TMS generates changes in synaptic plasticity, which ensures a prolonged effect7. Of course, this requires precise stimulation patterns, applied in specific protocols that can trigger a real response on the plasticity of the neurons.
The first step of rTMS (which has demonstrated real therapeutic effects) was to overcome the effectiveness of conventional treatments of refractory patients, such as electroconvulsive therapy. rTMS was first used in 1993 as a treatment for major depression in refractory patients8. After overcoming that first step, more in-depth and descriptive research was proposed on the various patterns and protocols that could be used in other diseases.
Neuronal Plasticity – The Secret of Long-term Effects
Research that has demonstrated the effects of rTMS on synaptic plasticity has focused on the primary motor cortex, although there are many studies related to depression and other psychiatric disorders such as anxiety and OCD.
According to these studies, depending on the intensity and direction of the current, it is possible to activate an entire pathway of neurons (such as the corticospinal tract) directly or trans-synaptically. We know from previous studies, especially animal-based studies, that repeated impulses through neurons can increase or decrease synaptic conduction in the long term, which is known as long-term “depression” (LTD) or “potentiation” (LTP).9
This is the basis for the short-term effect of rTMS. By increasing the intensity of rTMS, we can generate changes in neurons, creating new synaptic interconnections that stimulate various receptors. The more intense and repeated the impulses, the longer the changes will last. However, in order to obtain definitive results, changes at the protein level are necessary.
This conclusion was supported by studies on rodent brains where it was revealed that there are changes at the molecular level which may be the basis of synaptic plasticity and the crucial effect of rTMS in humans9. According to the available data, there are not only changes in synaptic structure (and neuronal interconnections), but also dynamic changes in calcium receptors, which modulate the expression of glutamate receptors10. Some data even show early gene changes that regulate the expression of previous genes.
In addition, there seems to be another method that can also affect synaptic plasticity, which is known as “spike-timing-dependent plasticity.” It is a kind of associative stimulation that has a fixed impulse (the conventional SMT) and the electrical stimulation of a peripheral nerve which carries its impulse to the cortex11.
Other mechanisms can also affect synaptic plasticity, however, the ones that have been most studied are the ones we have discussed above. Still, we cannot rule out the impact of rTMS that has even had effects on the neuroendocrine system by lowering cortisol levels in rats. Data are somewhat sparse on its effects beyond synaptic plasticity; nonetheless, it is really promising.
Approaches: rTMS as a Therapy
The effects of rTMS usually last about 30-60 minutes in humans, depending on protocols and usage patterns, such as pulse number, rate and intensity12. Of course, if this were the only effect, rTMS would not make real sense. Permanent changes (or at least longer duration) are crucial for using it as a therapy.
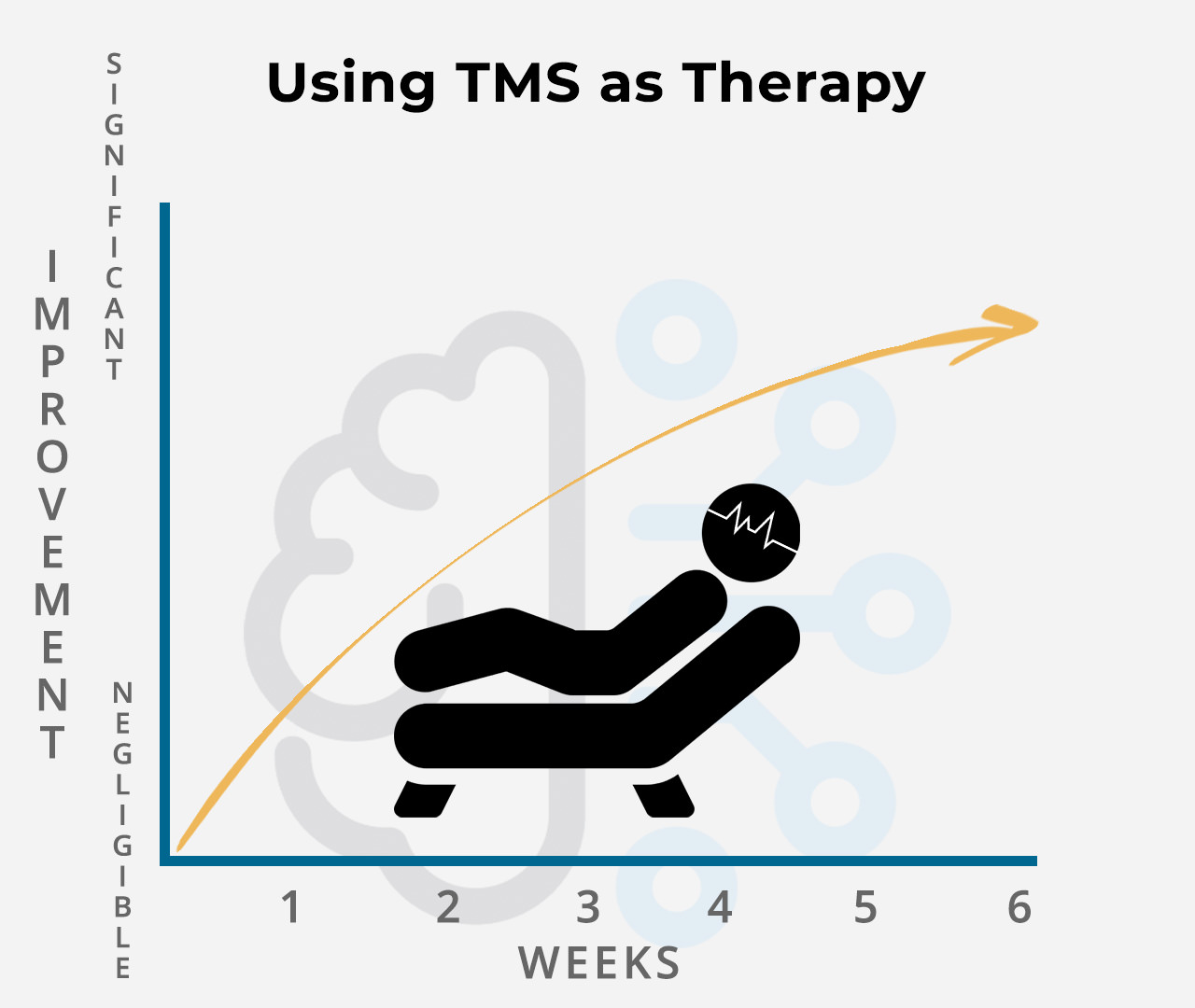
Repeated induction of plasticity seems to fill that gap by creating temporary changes for a long time (LTP/LTD). This seems to depend on the number of sessions, so protocols of 10 or more days of use (once a day) are often applied. So far, depression (for example) may warrant therapies of up to six weeks, at least 20-30 sessions for best effects13. The idea is to create structural and functional changes gradually, to “regularize” the neuronal interconnections.
In order to apply rTMS, the patient must be seated or in a “relaxed” position, in a comfortable environment. Some even consider using rTMS prior to physical or psychological therapy, which seems to cause dramatic changes and increases its effectiveness dramatically14. We will discuss the pathologies where rTMS has proven to be effective, going deeper into their theoretical bases and the various studies that corroborate these data.
Major Depression
Major depression is a worldwide health problem. Much attention has been given to mental disorders in recent years, yet the management of this illness remains a challenge, even for experienced clinicians. The idea of using TMS as an antidepressant has been around for a very short time, yet it has made great strides.
Most of the available scientific studies that have looked at the potential for TMS in major depression have yielded promising results, and there are always at least moderate changes in symptoms. There have even been studies with follow-ups of up to one year, where the results remain positive15.
Still, many parameters need to be adjusted to optimize the antidepressant effects of rTMS. For example, it is necessary to make precise calculations about the intensity used based on the scalp-to-cortex distance. It is necessary to find a methodology that provides accurate measurements.
Antidepressant Mechanism
The pathophysiology of depression is based on alterations in the effect of neurotransmitters on the various circuits of the brain. Some claim that both dopaminergic and serotonergic pathways are affected during depression. However, several studies have shown that TMS can increase dopaminergic transmission in both cortical and subcortical areas15.
Depolarization caused by repetitive therapy with TMS causes physiological and functional alterations of these affected brain regions, including the prefrontal cortex, which appears to play an interesting role in depression15. Moreover, let us remember that the effect is twofold, both direct and indirect, since the stimulus is also transmitted through the neuronal circuits.
It seems that when TMS is applied, it is possible to regulate the neurocircuits related to mood. If the appropriate intensity and frequency are used, it is possible to regain the lost balance of the brain waves. Also, although it has an activating effect on that mood circuitry, it may have inhibitory effects on cortical and subcortical networks related to the amygdala, an area of the brain linked to anxiety and fear, the mainstays of depressive episodes.
Movement Disorders
Several structures of our central nervous system are necessary to move; perhaps the most important are the primary motor cerebral cortex (M1) and the basal ganglia. Many movement disorders have some impact on the basal ganglia since it is the interconnection point of many structures (thalamus, cerebellum, cerebral cortex, etc.).
However, as mentioned above, the direct effect of TMS is quite small: it only reaches the cortex and part of the subcortical region of the brain. Even so, the secret lies in the indirect effect through the neuronal interconnection. The same stimulus received by the cortex can secondarily influence the basal ganglia circuit and produce demonstrable clinical benefits.
This idea has been confirmed with thousands of objective, theoretical, practical, descriptive studies, etc. Many use functional MRI to demonstrate how TMS can increase signaling and regularize the function of key structures in motor functioning, such as the thalamus and the striated nucleus. Some even used PET (more specific imaging studies) and confirmed the release of dopamine, which is often lacking in many neurodegenerative disorders.
Although there are many movement disorders, we will explain the focus and effect of TMS on the most common ones. Remember that almost all of them are due to important genomic alterations, so the treatment always ends up being palliative (symptomatic control) and not curative.
Among these we have:
Parkinson’s Disease
The basis of the physiopathology of Parkinson is the alteration in the production of dopamine in the basal ganglia, therefore the effect of rTMS is useful. Many studies have focused their efforts on determining this premise, and the results have been excellent16,17.
Unlike other diseases, such as Depression, rTMS protocols (high or low frequency) varied, so they provided mixed results. However, based on specific scales to determine the degree of motor impairment (such as the Unified Parkinson’s Disease Rating Scale, UPDRS), there was a significant overall improvement in all motor symptoms, including bradykinesia, temblor, stiffness, instability, etc.
The best studies used frequencies 1-5 Hz, significantly improving UPDRS. The effect was more pronounced than using slower frequencies (0.2Hz), especially when applied to the pre-supplementary motor area (SMA), which has a relevant side effect on the thalamus and the striated nucleus, which are fundamental in motor control.
Stimulation has been tested on other cortical areas, such as M1, which have also had a positive overall motor UPDRS impact, on stiffness and bradykinesia, but not on other motor parameters. In addition, areas such as M1 benefit from higher frequencies (10-25 Hz). The effect even exceeds that of the medication used for Parkinson’s18.
Huntington’s Disease
Analyzing the population with Huntington’s is more difficult because of the few existing cases (compared to Parkinson’s). The only studies that have tested rTMS on patients with Huntington’s disease analyzed the effect on SMA, which seems to play a crucial role in motor control during the onset of the disease19.
Here again, low frequencies (close to 1Hz) were used, which decreased involuntary movements. However, higher frequencies (5hz) were not shown to have the same effect, so further and more direct studies are needed.
Essential Tremor
Essential tremor is a pathology of which we know little. The physiopathology remains a mystery, hence the name “essential,” although genetic alterations and certain changes at the level of the cerebellum and other structures related to fine motor control (thalamus – motor cortex) are linked.
To calm the tremor, rTMS was attempted on the cerebellum, yielding various results. The best studies showed positive effects for more than three weeks with the application of five sessions (five days, once a day). This encourages further prospective studies with more follow-up20.
Obsessive-Compulsive Disorder
Obsessive-Compulsive Disorder (OCD) is a common mental disorder affecting more than 2% of the world’s population. This condition often occurs in conjunction with other illnesses such as anxiety and depression. Moreover, like all other psychiatric disorders, it is still very underdiagnosed.
As with the other pathologies mentioned, there are two effects of rTMS on OCD: direct (local) and indirect (secondary). The local effects of rTMS, especially on the motor system, are the most studied since it is the most accessible system for this therapy and allows objective measurements.
When someone has OCD, it seems that the brain circuits have variable activity, which plays an important role in rTMS. It is difficult to choose the cortical site of action, as well as the patient’s state during the intervention (doing some mental activity or resting). In fact, rTMS had proven its effectiveness and positive and promising results, but it is necessary to determine the pattern of brain activity of the OCD patient prior to intervention21.
Apparently, neuroimaging in conjunction with computer models and rTMS itself (acting as a diagnostic method) may help identify the brain circuits that should be targeted. The effectiveness of rTMS is not in doubt; it depends on how personalized the therapy is.
Should We Be Concerned About Safety?
As we mentioned from the beginning, rTMS is a fairly safe, noninvasive, controlled therapy that does not cause dangerous adverse effects. However, some published safety guidelines, among the most critical, have found certain complications to be rare but worth noting.
It appears that, in some cases, rTMS may inadvertently cause seizures in some people undergoing this therapy. However, this finding was made in patients who underwent rTMS through a safety study, using motor-evoked potentials beyond the area of stimulation. Therefore, this study should not be considered definitive.
In addition, there were some disturbances that attracted attention. For example, one of the seizures was induced with stimulation trains at excessively short intervals. Although the frequency and intensity were within safe limits, there was not enough time. The rule of thumb is that there is at least the same amount of stimulation time as space between sessions.
Finally, only 12 cases were reported from 1985 to 2003, a very low number for the thousands of studies conducted since that time. All this leads us to conclude that rTMS is a fairly safe therapy that has no real adverse effects known so far, so it can be freely used, as long as it is within the safety parameters established in the therapeutic protocols.
Limited Effectiveness and Future Directions
Although the information we have is quite promising and points towards drastic positive changes, we need more data and studies that support and provide new perspectives on rTMS as a therapeutic tool. The major limitation is how little we know about the mechanism of action of rTMS and what are the molecular steps that provide its benefits.
For example, the data supporting the use of rTMS in Parkinson’s patients are very promising, but why does it not work in the same way in pathologies with the same physiopathological mechanism? Why does it not have the same effectiveness in other diseases with dopamine deficit, such as depression?
In the case of movement disorders, we can assume that we have precise information about the specific area where rTMS can be used, whether it is M1 or SPA, but what about depression? Are there no other more effective regions where we can apply this therapy? The bottom line is that most studies focus on a single area while investigating depression, and there are still thousands to investigate.
It is even necessary to consider the anatomical difference of each person. We are all different and cortical areas vary slightly in position, thickness changes (bone, cortical and subcortical area), amount of tissue varies, etc. There are millions of variables that we still do not control.
We are barely understanding what the various patterns and protocols are that we can use, but the possibilities are almost infinite with rTMS. We need large-scale studies, which allow us to combine patterns and create comparative groups to follow them over long periods. The information is concise and promising but needs to be expanded and deepened.
Still, we know we’re taking the right steps. Major organizations like the FDA have approved the use of rTMS for depression and even obsessive-compulsive disorder22, which means that the positive effect and benefits of this therapy are indisputable. Soon, new diseases will be studied and the accepted therapeutic range of rTMS will surely increase.
Video: How Does TMS Work?
References
- Penfield W, Perot P. The brain’s record of auditory and visual experience: a final summary and discussion. Brain 1963;86:595. DOI: 10.1093/brain/86.4.595
- Penfield W, Jasper H. Epilepsy and the functional anatomy of the human brain. Boston: Little, Brown and Company; 1954.
- Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet 1985;1(8437):1106-1107. DOI: 10.1016/s0140-6736(85)92413-4
- Edwards MJ, Talelli P, Rothwell JC. Clinical applications of transcranial magnetic stimulation in patients with movement disorders. Lancet Neurol 2008;7(9):827-840. DOI: 10.1016/S1474-4422(08)70190-X
- Barker AT. An introduction to the basic principles of magnetic nerve stimulation. J Clin Neurophysiol 1991;8(1):26-37. DOI: 10.1097/00004691-199101000-00005
- Day BL, Dressler D, Maertens de Noordhout A, et al. Electric and magnetic stimulation of human motor cortex: surface EMG and single motor unit responses. J Physiol 1989;412:449-473. DOI: 10.1113/jphysiol.1989.sp017626
- Rothwell JC. Techniques and mechanisms of action of transcranial stimulation of the human motor cortex. J Neurosci Methods 1997; 74(2):113-122. DOI: 10.1016/s0165-0270(97)02242-5
- Hoflich G, Kasper S, Hufnagel A, Ruhrmann S, Moller HJ. Application of transcranial magnetic stimulation in treatment of drug-resistant major depression: a report of two cases. Hum Psychopharmacol 1993;8:361-5.
- Bliss TV, Cooke SF. Long-term potentiation and long-term depression: a clinical perspective. Clinics (Sao Paulo) 2011;66(suppl 1):3-17. doi: 10.1590/S1807-59322011001300002
- Mix A, Benali A, Funke K. Strain differences in the effect of rTMS on cortical expression of calcium-binding proteins in rats. Exp Brain Res 2014;232(2):435-442. DOI: 10.1007/s00221-013-3751-6
- Stefan K, Kunesch E, Cohen LG, Benecke R, Classen J. Induction of plasticity in the human motor cortex by paired associative stimulation. Brain 2000;123 Pt 3:572-584. https://doi.org/10.1093/brain/123.3.572
- Cirillo G, Di Pino G, Capone F, et al. Neurobiological after-effects of non-invasive brain stimulation. Brain Stim 2017;10(1):1-18. DOI: 10.1016/j.brs.2016.11.009
- Milev RV, Giacobbe P, Kennedy SH, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 4. neurostimulation treatments. Can J Psychiatry 2016;61(9): 561-575. DOI:10.1177/0706743716660033
- Bolognini N, Pascual-Leone A, Fregni F. Using non-invasive brain stimulation to augment motor training-induced plasticity. J Neuroeng Rehabil 2009;6:8. DOI: 10.1186/1743-0003-6-8
- Philip G Janicak and Mehmet E Dokucu. Transcranial magnetic stimulation for the treatment of major depression. Neuropsychiatr Dis Treat. 2015; 11: 1549–1560. doi: 10.2147/NDT.S67477
- Khedr EM, Farweez HM, Islam H. Therapeutic effect of repetitive transcranial magnetic stimulation on motor function in Parkinson’s disease patients. Eur J Neurol 2003;10(5):567-572. DOI:10.1046/j.1468-1331.2003.00649.x
- Ikeguchi M, Touge T, Nishiyama Y, Takeuchi H, Kuriyama S, Ohkawa M. Effects of successive repetitive transcranial magnetic stimulation on motor performances and brain perfusion in idiopathic Parkinson’s disease. J Neurol Sci 2003;209(1-2):41-46.
- Brys M, Fox MD, Agarwal S, et al. Multifocal repetitive TMS for motor and mood symptoms of Parkinson disease: a randomized trial. Neurology 2016;87(18):1907-1915. DOI: 10.1212/WNL.0000000000003279
- Groiss SJ, Netz J, Lange HW, Buetefisch CM. Frequency dependent effects of rTMS on motor and cognitive functions in Huntington’s disease. Basal Ganglia 2012;2(1):41-48. DOI: 10.1016/j.baga.2011.12.001
- Gironell A, Kulisevsky J, Lorenzo J, Barbanoj M, Pascual-Sedano B, Otermin P. Transcranial magnetic stimulation of the cerebellum in essential tremor: a controlled study. Arch Neurol 2002; 59(3):413-417. DOI: 10.1001/archneur.59.3.413
- Luca Cocchi, Andrew Zalesky, Zoie Nott, Geneviève Whybird, Paul B. Fitzgerald, and Michael Breakspear. Transcranial magnetic stimulation in obsessive-compulsive disorder: A focus on network mechanisms and state dependence. Neuroimage Clin. 2018; 19: 661–674. doi: 10.1016/j.nicl.2018.05.029
- U. S. Food & Drug Administration. FDA News Release. FDA permits marketing of transcranial magnetic stimulation for treatment of obsessive compulsive disorder. August 17, 2018. Retrieved from https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-transcranial-magnetic-stimulation-treatment-obsessive-compulsive-disorder
STOP TAKING MEDICATIONS
No More Ineffective Drugs
No More Debilitating Medication Side Effects
HEAL YOUR BRAIN
Increased Brain Cell Activity
Increased Brain Cell Connectivity
Increased Brain Plasticity
SIMPLE TREATMENT PROCESS
Non Invasive
No Anesthesia Or Medication
No Side Effects
Immediately Resume Normal Activites
Conditions Treated
We utilize the most advanced Transcranial Magnetic Stimulation technology available to provide healing for an extensive range of mental and neurological conditions, without medication, discomfort, or side effects.
TESTIMONIALS
Read about the experiences that recent patients have had with TMS
Debilitating Depression
“After I don’t know how many different medication prescriptions, none of which worked like they should, I tried TMS because I couldn’t continue to live with my depression. The result has been really miraculous. I feel so much better, now. I feel more capable of doing things. I’m so much happier. TMS has been a savior to me.”
Anxiety Attacks
“I experienced anxiety attacks since I was a teenager. I’ve tried anti-anxiety medications, along with all of the other medications that I was taking, but they didn’t help with my panic. I found myself unable to function – I would completely spiral inside myself, hanging on for my life when the attacks would come. I had hear about TMS from someone. I was desperate and didn’t have anything to lose, as nothing was working. Dr. Schneider and Art are both terrific. They made me feel so comfortable and educated about TMS. I must say that initially I didn’t feel a big difference. But I knew that it often takes many sessions for the effects to occur for some people. I was one of those. But I cannot be more pleased with the improvement in my attacks. I feel so much more in control and calm. I am becoming, who I used to be, when panic and anxiety didn’t rule my life. I know that it will only continue to improve. I highly recommend TMS.”
Daughter’s ADHD
“TMS changed our daughter’s life. She was diagnosed with ADHD in second grade. We took her to child psychiatrists and tried numerous medications, and therapy, but none of it had any real positive effect, as her symptoms only increased over time, to the point where she was failing in school, and had considerable difficulty with tasks outside of school. We had heard about TMS and we decided to try it, although we did not have great faith in it. But we were amazed. After just a few sessions, we noted improvement in our daughter. She was able to concentrate on school work, specifically math, for the first time, ever. She doesn’t need all of the stimuli, anymore, that she used to need (phone, TV, music, computer all on at the same time) just so that she could feel ‘comfortable’. We are seeing improvements every week, in her behavior, her level of calmness, her interactions. It is truly amazing. So far, extremely good. We are believers in TMS.
TMS Information and Consultation
SAN DIEGO LOCATION
Schedule Consultation
View Videos
FAQ
Patient Forms





















